- Using the primary assessment framework: Outline the expected signs and symptoms of COPD with linkages to underlying pathophysiology.
C – It is possible for severe COPD to cause cardiac complications and respiratory arrest due to decreased oxygen supply (resulting from narrowed bronchi and poor O2 uptake from damaged alveoli and decreased lung compliance) and chronic inflammation (Vandenberg et al., 2016). If the patient presents without a pulse, it is recommended to start CAB (circulation/ chest compressions, airway, and breathing) to help restore tissue perfusion and oxygen supply.

A – If the patient is unconscious, assess their airway. Depending on the severity of the COPD and level of exacerbation, the patient’s airway may be compromised due to narrowing of the bronchi and excessive mucus (Lewis et al., 2019).
B – Due to increased airway resistance and decreased lung compliance, work of breathing is usually elevated in patients with COPD (Lewis et al., 2019). Dyspnea is also present due to an increased residual lung volume resulting from the reduced ability to expire air. Dyspnea is usually more evident on exertion (due to the higher oxygen demand), but may also be present at rest in more severe cases. A productive cough may also be present due to excessive mucus production (due to chronic lung inflammation). Because of this, coarse crackles can usually be heard on auscultation. Wheezing may also be present due to the narrowed bronchi (Lewis et al., 2019). Low oxygen saturation is a common symptom due to alveolar hypoxia. If the SpO2 gets too low however, it may cause cyanosis or alterations in level of consciousness due to inadequate perfusion. At this point in the assessment, it would be wise to apply supplemental O2 therapy in an exacerbation of COPD (see section #2 “Oxygen Supply and Demand” and section #3 “Interventions” for more information).

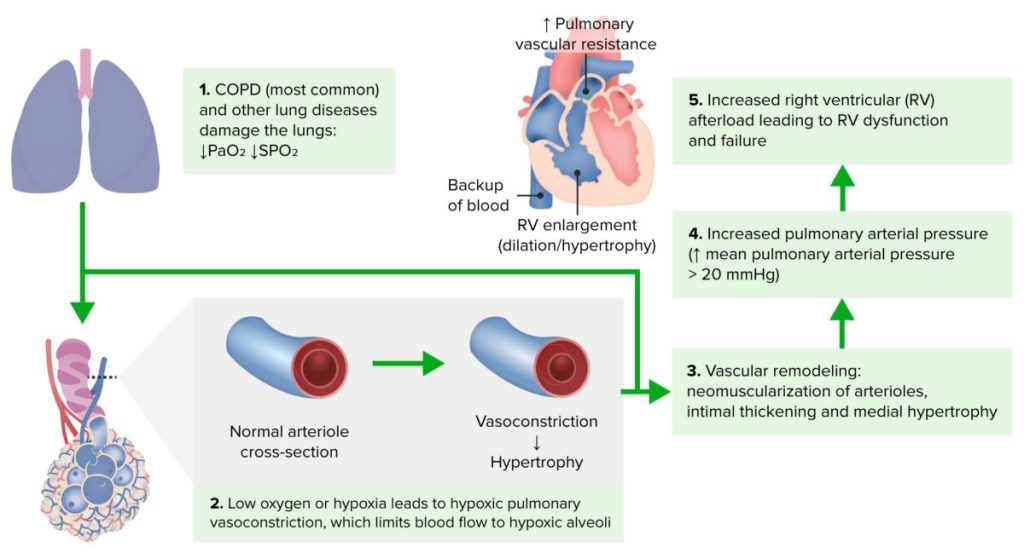
C – Circulation may be impaired in COPD patients. Pulmonary blood vessels may become narrowed/ blocked due to excessive strain which causes pulmonary hypertension. This can result in cor pulmonale which can cause an irregular heart rate and edema. COPD can also result in tachycardia due to chronic hypoxia (Lewis et al., 2019). COPD may also result in cyanosis due to inadequate tissue perfusion and oxygen supply. Chest pain may be present due to respiratory muscle strain.
D – Assess AVPU (Is the patient alert? Responsive to verbal stimuli? Only responsive to pain? Unresponsive?). If AVPU is abnormal, then assess the patient with the Glasgow Coma Scale (GCS) and PERRLA (pupils equal, round, reactive to light and accommodation) to assess for neurological impact (Lewis et al., 2019).
D – As Mirrakhimov (2012) discussed, COPD exacerbations can cause the patient to become hyperglycemic. This is because of the release of cytokines which causes insulin resistance and, consequently, hyperglycemia. Because of this, it would be wise to assess the patient’s blood sugar if they present to an emergency department. The patient may be in pain/ discomfort from respiratory muscle strain and high WOB, potentially requiring pharmacological support before the primary assessment can be finished (see section #4 “Medications” for more information). It would be important to notify a physician so that they could write an order for a relevant medication and be aware of the patient’s status.
E – Expose: Ask the patient to change into a gown. Depending on the severity of the COPD, it may be possible to see accessory muscle usage when breathing (to help with ventilation which is impaired in COPD due to the narrowed bronchi and mucous production). Peripheral edema may be present due to pulmonary hypertension (resulting from narrowed/ blocked pulmonary blood vessels) leading to cor pulmonale which causes blood/ fluid to back up in the body (Lewis et al., 2019).
F – Take a full set of vital signs to assess severity of exacerbation. Respiratory rate is usually increased as a compensatory mechanism of respiratory acidosis (resulting from hypoxia and hypercapnia). Tachycardia and hypertension are also usually present due to tissue hypoxia which activates the sympathetic nervous system (Mahmoud et al., 2016). Body temperature may be within normal range in patients with COPD, but in an acute exacerbation a fever may develop secondary to a respiratory infection. As discussed under section “B”, SpO2 saturation will be decreased due to inadequate gas exchange from alveolar damage (Lewis et al., 2019).
F – Ask if there are any family present and if they or the patient has any questions.
G – Go back and reassess. Supplemental O2 therapy should have been applied to help with the patient’s dyspnea (Lewis et al., 2019). Assess if the amount or delivery of oxygen needs to be adjusted before moving to the secondary assessment. Pharmacological interventions may be required in an acute exacerbation of COPD to provide the patient with more noticeable relief (Lewis et al., 2019) (see section #4 “Medications” for more information on appropriate medications).
References:
Lewis, L., Bucher, L., Heitkemper, M., Harding, M., Barry, M., Lok, J., Tyerman, J., & Goldsworthy, S. (2019). Medical-surgical nursing in Canada (4th ed). Elsevier Canada Ltd.
Mahmoud, K., Kassem, H. H., Baligh, E., ElGameel, U., Akl, Y., Kandil, H. (2016). The effect of ivabradine on functional capacity in patients with chronic obstructive pulmonary disease. Clinical Medicine. 16(5), 419-422. https://doi.org10.7861/clinmedicine.16-5-419
Mirrakhimov, A. E. (2012). Chronic obstructive pulmonary disease and glucose metabolism: A bitter sweet symphony. Cardiovascular Diebetology. 11(132), 34-60. https://doi.org10.1186/1475-2840-11-132
